You’re invited on Thursday, April 13, 6:30 to out beloved local independent bookstore, Eagle Harbor Books, Bainbridge Island.
https://www.eagleharborbooks.com/event/jeannette-franks-phd-shares-her-book-intentional-aging
Gerontologist, Author and Activist

You’re invited on Thursday, April 13, 6:30 to out beloved local independent bookstore, Eagle Harbor Books, Bainbridge Island.
https://www.eagleharborbooks.com/event/jeannette-franks-phd-shares-her-book-intentional-aging

Aging well is achievable–if you know how. And I can teach you how in the 7 concise chapters in this book. You will learn how to avoid dementia; how to maximize your finances; how to document your end-of-life choices; how to modify a home for you to age in place; and how to age well with purpose and joy.
from the book: “There are many excellent books on home modifications for aging in place. There are books and more books on end-of-life issues. There are books and books and books on exercise! So why read this particular book? Read this book because it brings together these most important issues in a concise, useful way. Why get four or five books on these seven topics when you can use just this one? I have worked to bring the most relevant current information to you in a succinct, readable way.”
in the worst of times and the best of times

Jeannette Franks, Aug. 25, 2021
The 2020-21 pandemic indelibly engraved on our collective psyches the importance of family, friends, and community support. It is intuitive that love, friendship, conversation, even conflict, are essential. In our later years a robust social safety net can not only mean the difference between life and death, but we also know that positive social support can contribute to a good life and a good death.
I am including in this big social support bucket not just relationships but governmental and societal life jackets. We sometimes take programs such as Social Security, Medicare, Medicaid, long-term care, Area Agencies on Aging, non-profits, and public health agencies for granted. Watch out! They are often threatened by new administrations, new administrators, and new legislation.
During the COVID crisis, many who were formerly contributors to food banks became recipients. Some agencies make the people they serve feel embarrassed and demeaned. Others do not. So, not only are social services often in jeopardy of negative changes, but services might be provided begrudgingly.
During the pandemic, at a time when those in my eligibility tier (70 and over) were struggling to find vaccine appointments, a member of my book group sent an email to all of us, announcing the availability of vaccine appointments at a hospital an hour away. We all signed up and were successful. So many seniors locally were struggling to get appointments that a non-profit that usually provided volunteers for transportation and other services, trained a cadre of volunteers to find appointments, notify and sign up those eligible, and set up transportation. This combination of personal networks and a well-organized non-profit is exemplary and effective.
On a human level we can individually and collectively nurture our personal relationships consciously. Think of ways to foster a sense of community in your neighborhood. What comes to mind? Backyard barbeques, joint garage sales, progressive dinners moving from one home to another one, a course at a time, consciously creating connection. In my condo we have a weekly social hour.
In my small town, for many neighbors the emergency preparedness process set up by our city introduced neighbors to each other and established life-long friendships. Partners in 43 states have used this “Map Your Neighborhood” disaster preparedness program. The website will pop up if you search for “Disaster Services and Supplies”. The detailed booklet covers what to do in earthquakes, heat waves, blackouts, tornedoes—the potential disasters list is huge. The official website did not at the time of this writing this include pandemics, but our city used the structure created by Map Your Neighborhood to recruit leadership, find and share emergency supplies, locate those in greatest need, plan for the future, and alert the community by emails and texts to quickly changing situations.
Structured social support consists of two distinct yet intertwined spheres. A nurturing community has both non-profit and for-profit agencies that respect and assist people of all ages, backgrounds, ethnicities, and incomes. A good community is an elder-friendly community.
The World Health Organization (WHO) has created guidelines that transcend countries and cultures. Ireland was the first to be recognized as an elder-friendly country. Montreal, Canada and Portland, Oregon and recognized as elder-friendly cities. A genuine age-friendly community has a competent Public Health Department, and in my opinion, health insurance for all. The pandemic has revealed many lacks in health care such as an initial shocking shortage of personal protective gear for front-line workers. Many communities responded by sharing skills and materials to sew masks from scratch.
An important factor in an elder-friendly community is safe, accessible, affordable transportation. While not all of the oldest-old are unsafe drivers, many are. Yet the lack of public transportation, especially in rural areas, is a huge barrier to giving up a car. In addition, many Americans identify independence with driving. Teenagers and those over 85 have the highest rate of accidents per miles driven. All age groups should be subjected to identical scrutiny. Perhaps we need comprehensive driving exam for every driver every 10 years?
No one policy has solved the demented driver dilemma. Every family figures out different strategies—or not. We told Dad that the car had been recalled and made sure he had plenty of other options to get where he wanted. Eventually he stopped asking when the car was coming back. I know some families that have disabled the vehicle. If one doesn’t have the mental and financial wherewithal to plan and execute car repair, it cuts down on dangerous drivers.
I attended a panel at a national aging conference on dangerous drivers. One organization had created a ‘driving advance directive’. The person in peril of being at risk in the future signed a document saying that he or she knew that at some time “I will be an unsafe driver” and designated a specific person to make that decision. The audience thought it was a brilliant idea until someone asked, “Did it work?” “No”, was the sad answer.
Not just Alzheimer’s, but many of the other dementias—Parkinson’s, stroke, Lewey bodies, brain tumors, reduce the ability to drive dramatically. Other age-related disabilities such as tremors, slowed reactions, stiffness to view side traffic, and more interfere with driving.
Most states have a protocol where physicians can report unsafe drivers. One hopes that when that is reported, some action is taken. There are even apps such as “Bad Driver Database” where you can use your phone to snap a photo of an unsafe driver and it at least creates a record. It isn’t clear again whether any action results from being reported. Some state Departments of Licensing have a form that can be used anonymously to have unsafe drivers evaluated. As an example, here is the link form for Washington state https://www.dol.wa.gov/driverslicense/reportunsafe.html.
Many cars now have back-up cameras as well as sensors around the entire car, warnings systems, automatic braking systems and more to help older driver. Those that can afford it may well benefit from a state-of-the-art car with maximum safety devices. The other vehicles on the road will be safer as well.
Any possible way individuals and communities can provide transportation will foster aging in place.
Getting unsafe drivers out of their cars can save lives, for example my 92-year-old neighbor who backed over and killed a grandmother in front of her horrified grandchildren.
Affordable, accessible housing is another factor that creates an elder-friendly community. Ideally, when new multiple-unit housing is designed, local data on what percentage of the population is of various ages and income are consulted. For example, a one hundred-unit apartment complex could reflect the percentage of older and/or disabled population and sell at a diverse range of prices. So, if 15%, (a likely figure in the US) is over 70 or disabled, 15% of the units are accessible, including a wheelchair-usable entry and bathroom. Permitting for new structures can include requirements of a certain percentage being low income and affordable. How many U.S. communities do this? Few, if any.
Negative social support
While it is easy to acknowledge that social support has positive value, we often have a hard time grasping that there is also the opposite—negative support. Think of those people who suck more from you than they return. Not all relationships are symmetrical, nor must they be. But those people who need so much—so much sympathy, so much help, so much listening, can drag you down. At what point is it harmful to you? How important is self-interest if you are truly needed?
Consider how much there is that can be sucked from you without damaging the nurturing you give others and that you give to yourself. Of course, relationships in our lives differ greatly and change over time. The same person can be primarily the listener in one relationship and the talker in another. But when it is noticeably unilateral over a long period of time, sometimes self-preservation sets in. Allow yourself, to say, “Sorry mom, I can’t come to dinner this week” or “Forgive me, Angela, I must hang up and take another call.” I’m not suggesting totally ghosting family members, unless it is an abusive relationship, but while blood is redder than water, it’s not always the best binding force.
It breaks my heart to have long-time friends that when you talk, it is totally one-sided. There are crises in all our lives. At these times you must receive the pain and sorrow from a dear friend, and listen, listen, listen. However, it can eventually return to a true conversation, in which each person listens and talks. An equal friendship is healthy.
Helping someone in grief here???
There is a myth in America that in the ‘good old days’ families (read ‘women’) took care of aging relatives, while now we are selfish and farm out older people to nursing homes. In reality, quite the opposite is true. As noted earlier, less than 5% of all people 65 and older are in a nursing home. Also, in the good old days, people died much younger. The life expectancy in 1900 was 50 for women and a bit less for men. In 2020 the average person can expect to live to be 80. Of course, many of those in their 70s, 80s, and 90s, need support and current data suggest that a majority of us will be caregivers and carereceivers at some point in our lives. The interdependence of humans is marvelous and productive. While we are a nation founded on a declaration of independence, in fact at all stages of our lives we give and receive interdependencies. An effort to foster interdependence is a normal and desirable state, even imperative.
The analogy of the equity of babies being dependent on parents and then parents becoming dependent on adult children is false. When babies are born, humans in general will learn to toilet independently, go to school, mature and support families themselves eventually. However, it is unlikely that a disabled 80-year old will ever get more independent rather than less, despite the wonders of surgery, physical therapy and medications.
Interestingly, the trend appears to be that, while we used to think of elders moving in with adult children, more often today adult children move in with their aging parents. Housing is crushingly expensive, as is homecare. There is social support in togetherness. But don’t forget the mantra of many a school of social work, “All families are dysfunctional.” To me, it is a question of degree and coping mechanisms. When you hear a complaint that “my kids never come to visit” ponder the possibility that this parent might have been abusive, physically or verbally, or both. Not every family is like Leave it to Beaver. In fact, sociologist Stephanie Koontz wrote a brilliant book called, “The Way We Never Were,” clarifying with research that blended families have always been the norm, and many families are dysfunctional to the point where that is also normal. She also points out, as just mentioned, that life expectancy was so low in the past that it was normal to lose a partner to death and then remarry. Divorce was uncommon because women had few rights. But it was normal to have more than one ‘life’ partner throughout a normal life. She calls it ‘serial monogamy’, which sounds like a delicious breakfast to me.
Holidays
The pandemic gave many families the opportunity to reconsider how and why we come together. Zooming replaced flying across the country for holidays. Various relationships appear to have been improved by distance. Skipping Thanksgiving with querulous cousins was easy! Faking unfelt piety unnecessary. Stressful guilt trips gone. Next year holidays may be more optional than obligatory. Think of creating new traditions with smaller carbon footprints and larger space for joy.
Celebrating the solstice has been traditional for at least a millennium. Traditions and rituals soothe stress. That may be why many risked life-threatening infection during COVID to gather with family and religious groups. Think about creating new traditions that fight isolation, promote happy harmony, and are happily anticipated rather than dreaded.
Pets
While tinder, Matchup.com and other web services make it easier and riskier than ever before to date, the unconditional love of a pet can soften the sorrow of loneliness. Dog and cat adoptions soared during the pandemic. And while it is challenging to manage the needs of a dog when working full-time away from home, there is an entire industry of dog-walkers, doggie daycare, and dog-friendly businesses. Tell an adorable story here.
An epidemic of loneliness
correlations with well-being. NYTimes May 15, 2020 “According to Gallup, Americans are experiencing the sharpest drop in perceived well-being on record.” While fear of death for oneself and for loved ones is part of that, isolation may contribute to a lower disease risk, but it does not enhance well-being. What indeed is perceived well-being? Write about relative deprivation
Other important connections are intersections that we may not recognize as vital, but help foster a sense of belonging and happiness. Those are those seemingly unimportant people with whom you come in contact in a normal day, or even during the pandemic. Think of the grocery workers who look you in the eye at your regular market and honestly ask how you are doing (and vice versa). The kindness of your mail carrier that you know visits your home every day is a little pleasant boost of sociability. Your hairdresser, your physical therapist, your neighbor sweeping her walk. Seemingly trivial conversations enrich our lives with information, humor, and kindness. A book entitled Consequential Strangers M. Blau and K. L. Fingerman researched these relationships with people not relations or close friends and found them they help with a basic human need for community.
Many of us became ‘zoomers’ during the pandemic and my instinct is that we will continue these electronic meetups even when the COVID epidemic is over. Zoom or whatever of the programs you use, both free and for a fee, combat not just loneliness and disconnection, but enable us to participate in meetings, conferences, friendships, and family ties that were inconvenient at best and impossible at worst. One branch of my dozens of cousins zooms every Saturday night. One neighbor video chats with her many sisters every Sunday. Our senior center has an 11:30 zoom every weekday with guest speakers, travelogues, talks on memoire writing, local organizations and more. I zoom quarterly with a statewide council on invasive plants and animals, which I find fascinating and useful. While I would never drive to our capital many miles away, I am delighted to virtually sit in on the briefings from all the experts.
Technical devices can aid connecting with family and friends: GrandPad may be worth the $200, but 8” isn’t very big. Several devices are meant to replace smaller, more complicated phones and larger, more complicated computers. These can be considerably cheaper than most phones or iPads.
The software and devices were used for memorials during the pandemic. It is so important for healing to have some type of ceremony. There is no right or wrong way to do, but evidence indicates that it is helpful to have a gathering, even if by phone, electronic notebook, or computer.
Acknowledging grief
One of the horrific hazards of choosing to work professionally with older people is that I repeatedly lose my mentors, my friends, my colleagues. Even worse, as I age, I lose more and more family to death. It is a reality. Losing a pet can also teach us that life is finite.
Over these many years of teaching about end-of-life issues, and personally losing so many of those dear to me, I have learned what is most helpful to say to those in grief.
When you learn that a person has lost a close friend or family member, particularly a beloved partner, please do not immediately change the subject and describe your saddest loss. This is not about you. It shows an incredible lack of empathy to try to offer sympathy by demanding it in return. A famous book on the subject is entitled Don’t Ask for the Dead Man’s Golf Clubs. A young widow with two children was appalled at such comments as, “You are still young enough to remarry.” Or, “He’s in a better place.” To her, a better place was alive by her side.
It is always correct to say, “I’m so sorry for your loss.” Or, “I can’t possibly imagine how you feel.” Because, of course, you cannot imagine how someone else feels, especially with the death of someone much loved. When my beloved husband died, it was agonizing how many people said, “Oh I remember how awful I felt when my husband, (wife, father, or whoever) died.” It put me in the position of saying, “I’m so sorry your whoever died.” While I was sad for their loss, I did not want their added sadness on of top on mine at that time.
There is no wrong or right way to grieve and no time limit to ‘finish’ grieving. Grief takes as long as it takes. I try not to judge a grieving person; while one can be sympathetic and empathetic, each loss is unique and personal. The three most important things you can do are listen, listen, listen. It is a great need of the bereaved to tell their story.
Losses that come unexpectedly, especially death to a younger person, can be especially difficult. It is heartbreaking to lose a parent, but in most cases even more tragic for a parent to lose a child. Compounded losses are also more difficult. To lose one beloved family member is horrendously hard. To lose multiple members of your family is crushing.
My opinion is that to some extent the demonstrations and some of the destruction that occurred during the pandemic were, in addition to anger at hundreds of years of systemic racism and abuse, also about the losses and resulting grief we were experiencing at that time. We lost our freedom to do normal activities, such as go to dinner and a movie. Many have lost friends or family to COVID. We appeared to have lost a functioning democracy for a time. We were grieving the disregard of truth and science. This grief, this anger and fury at injustice and racism, the horrible history of slavery and injustice, were being publicly expressed. There is hope for healing when the depth and profundity of these factors is better understood and addressed.
The paragraph above was written before the bizarre destruction at the Capitol Building in Washington DC on January 6, 2021. While there is no rational explanation of why Donald Trump would encourage people to riot and invade the Capitol Building, I suggest that his followers responded to his mad urging partly because of the grief, stress, and pain of the pandemic. It well might have been, to a certain extent, a manifestation of dysfunctional grief.
Often complicated losses such as sudden or multiple deaths result in dysfunctional grief. What does functional grief look like? Extreme sadness. But dysfunctional grief often shows itself as drug or alcohol abuse, family abuse, blank stoicism, fury—what else? The Native Americans in this country lost countless family and friends, first to diseases to which they had no resistance, then to the so-called “Indian Wars” and forced relocation. They lost their land, their sources of food, their culture, their languages, their religions, and most tragically, their children. All over this country children were taken from their indigenous parents and sent to ‘boarding schools’ where they were forced to abandon their loved ones, their clothes, even, most cruelly, their languages. Many were physically abused with forced labor and sexual abuse. Experts suggest that these multiple, unresolved, and egregious losses have resulted in manifestations of dysfunctional grieving.
Dealing well with loss is immensely helped by positive social support at all levels. Fostering strong positive relationships provides huge benefits for heath, happiness and longevity.
The entire issue of the December 2020 AARP bulletin is dedicated to multiple articles and perspectives on the horrific loss of life to COVID in the U.S. nursing home industry. And believe me, it IS an industry. Seventy percent of all skilled care facilities (the licensing nomenclature of ‘nursing homes’) are for-profits.
https://www.aarp.org/caregiving/health/info-2020/covid-19-nursing-homes-an-american-tragedy.html
While many researchers, experts, and workers in long-term care long saw it as a disaster, not just waiting to happen, but actually happening throughout their history, it took massive loss of life to get the journalists, politicians, workers, to put nursing home fatalities on the front page.
“Fewer than 1% of Americans live in long-term care facilities. But 40% of COVID-19 deaths have occurred there” (AARP.org/bulletin 12/2020). Within four months of the first known infection, some 54,000 residents and workers in long-term care facilities died of causes related to COVID.
There is finger-pointing every which way. Lack of personal protective equipment, lack of availability of timely testing, too many residents per staff, poor infection control, and lock downs that kept long-term care ombudsmen from seeing what was actually happening.
Blame goes back to the 50s with misguided laws that ultimately made nursing homes, “The bastard child of the poor house and the hospital,” the late Rosalie Kane, Ph.D., revered expert on long-term care.
According to the AARP special edition, we wound up with a medical model of a crowded hospital, as opposed to, for example, a college dorm or a modest hotel. Forcing frail folks into small multiple-occupancy rooms with beds four feet apart is a petri dish for disease. If it were not for the pandemic, many people would not have foreseen the disaster predicted by experts for decades. In addition, one expects to spend a few days or at most a few weeks in a hospital. To live a life lacking in privacy, autonomy, and choice for months or years is cruel.
Many facilities have long been understaffed and underfunded. “For-profit structure appears to have reduced quality at many nursing homes.” The funding structure, with three-fifths of residents paid for by Medicaid, doesn’t make for a balanced budget. “The relatively small number of well-paying (private pay) residents make up for the money they say they lose on the rest.”
As I have ranted elsewhere, we needed a total transformation of long-term care into one that is person-centered, affordable, homey, and respects individuals, caregivers, and families.

 The two foci of my life are: mitigating global warming and improving long-term care. These are related, because both are essential quality of life issues.
The two foci of my life are: mitigating global warming and improving long-term care. These are related, because both are essential quality of life issues.
COVID itself is related to global warming because as habitat for bats and other wildlife decreases, human/wild creature interactions increase, to the detriment of both. Restoring native plant habitats all over the world will do a great deal to slow down warming and potentially decrease the chance of pandemics from interactions with and consumption of wild creatures. Plus, intact forests are one of the more gigantic carbon sinks on this planet.
Greening long-term care also has the potential to minimize the risks of COVID for both workers and residents of nursing homes, which have suffered 40% of the incidence of COVID in this country and one of the highest rates of mortality so far (Winter 2020). By greening I refer specifically to “Green House” homes, the brilliant model created by Harvard-trained MD Bill Thomas. Who among us wants to live in a small double-occupancy room with a stranger and a shared bathroom? Not only is this a recipe for conflict (particularly if dementia is involved), it’s also a petri dish for COVID and any other infection you can think of.
For decades my fellow gerontologists and other experts in this field have worked for improvement of nursing homes by teaching and action to create smaller, more homelike settings where staff and residents have real relationships. The Providence Mount St. Vincent in Seattle created this, even with a huge facility, by creating ‘neighborhoods’ on each floor with a small group of residents in rooms around a central dining, living, and hanging out area. Dr Thomas’ model involves small groups of eight to 10 in group homes with private rooms around a central kitchen, dining, and relaxation area. Variations abound, but the key is intimacy, relationships, and a physical and emotional sense of home. Washington Post (11/3/2020) did an insightful article about this https://www.washingtonpost.com/local/green-house-nursing-homes-covid/2020/11/02/4e723b82-d114-11ea-8c55-61e7fa5e82ab_story.html. With the right reimbursement from Medicare and Medicaid, as well as increased respect for the elderly and the workers who help them, it can be cost-effective. Ageism and racism are part of the reason most people haven’t even heard of this model. Our society has disrespected the immigrants, the women, the people of color who dominate caregiving, and we’ve disenfranchised older people as a culture as well.
I think with our new administration coming in January we may be able to do more about this. Systemic racism is no longer acceptable and distain for older people and their caregivers is on the wane.
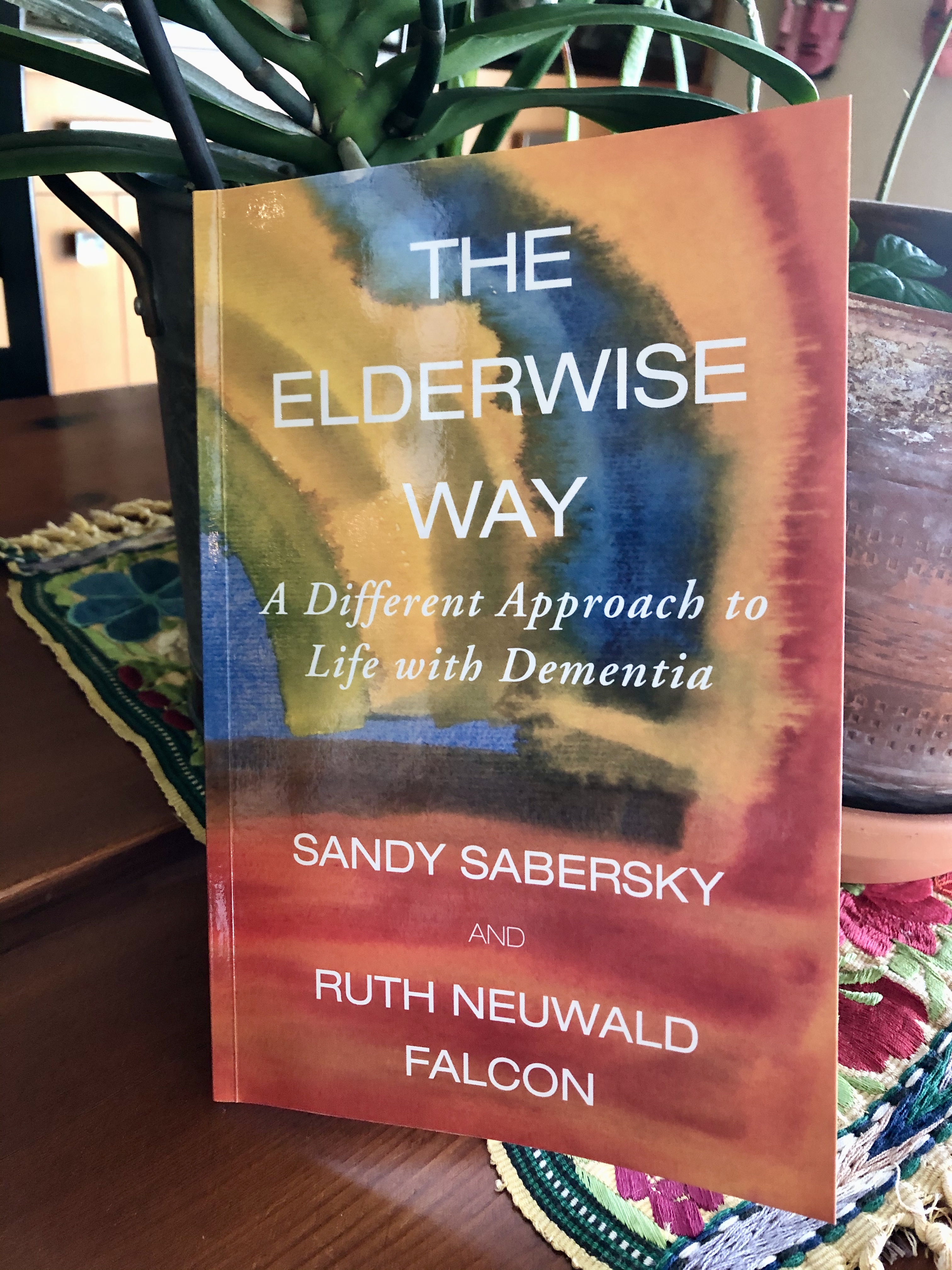
Review of The Elderwise Way, Sandy Sabersky, available on Amazon
People with Alzheimer’s can live a life of anxiety, sadness, and pain. Or people with dementia can live a life of joy and beauty. You will increase people’s chances of the latter if you read this book.
Compassion is at the core of all the world’s major belief systems: Buddhism, Islam, Judaism, and Christianity. “Do unto others as you would have them do unto you.” Compassion is also the heart and core of her brilliant new book, The Elderwise Way, and the Elderwise programs.
The author describes the Elderwise day: where one is warmly welcomed with delight; seated comfortably with a warm beverage in a mug and toast at a table with fresh flowers or natural items such as shells or lovely stones. Then you are invited by a facilitator to talk or be quiet. Toward the end of the social hour the participants transition to paint or work with clay or poetry; then there are moments of meditation and guided movement with music; then a delicious freshly-cooked healthy lunch.
Heck! I wish all of our mornings started and ended this way! While the author mentions that all people should be treated as of equal value, much like Mr. Neighbors, “you are perfect just as you are,” we should all be reminded that this holds true for all people of all ages, not just ‘elders’.
You need not be a location-based entity to honor people the Elderwise way. Nor do you even need to be an elder or caregiver. Read this book and learn the how and why of better treatment of people of all ages and cognitive states. Buy this book or request it from your local library. As a writer myself, I know the agonizing suffering of birthing a book. It should not go unread!
Jeannette Franks, PhD
I wear two hats. One hat is that of a PhD gerontologist specializing in long-term care, alternatives to nursing homes, and aging well. The other hat is as an award-winning expert on native plants and habitat restoration. They are related in an intricate web on our suffering planet. Nursing homes in the US and Europe have been particularly hard hit by COVID-19.
“Weed Warriors are not ornamental gardeners. Noxious weeds are not about dandelions. Read on!
What does a healthy native plant environment have to do with global warming? It has everything to do with global warming, not to mention COVID-19, and quality of life for humans of all ages and all living things.
As I write this in August of 2020, the U.S., ostensibly the richest country in the world, has one of the 3 highest rates of COVID-19 per capita in the world. In addition, the virus has killed Black Americans at twice the rate of others in the country. Older people are at greater risk of contracting the virus, dying from COVID-19, or being left with lasting disabilities. The issue of global warming is connected to the corona virus in multiple ways. As habitat shrinks from rising seas and encroachment of human habitation and farming, wild creatures, such as bats, lions, rats, and the viruses, bacteria, and dangers they spread, will increasingly invade human habitations.
How can we green the planet to insure a decent world for our grandchildren and our species?
We can restore the environment around us to a more natural state. When we clear-cut forests for farms, or cities, or timber, the first plants that appear are non-native noxious weeds. These invaders can smother the more productive and desirable plants with aggressive growth, stifling the trees that help combat global warming.
Weed Warriors struggle on Bainbridge Island to return parks, forests, road ends, schools, tree farms and the like to a more natural, healthy, sustainable environment. Trees are a priority, and trees are on the front lines of global warming. I could go on about the healing qualities of green and nature, but this is a start on understanding why removing ivy, Scotch broom, tansy ragwort and other noxious weeds is important, gratifying, and fits into a larger context.
As I write this in spring of 2020, we are seeing deaths and diagnoses of coronavirus climb. This may be the worst health disaster since the plague in the middle ages. It is yet another reason to stay out of a nursing home. A Seattle area skilled care facility was the epicenter for Washington state, which was one of the three hardest-hit states in the country early in the disease. The CDC found that a staff member in that nursing home worked two different days with symptoms, which then promptly spread to 82 residents. While the death toll continues, the first facility infected had 160 people sickened and 35 who died of COVID-19 as of February 2020. Two of the same hands-on staff there also worked at two different facilities, spreading the virus among staff and residents quickly. Nursing home caregivers often work more than one job in order to support themselves and their families. The CDC investigation also found seven people at the facility who were infected but showed no symptoms at the time. Cited from Seattle Times March 26, 2020.
According to the April 15, 2020 New York Times, “Virus deaths at U.S. nursing homes top 3,800, with 45 at one site in Virginia.” The Times included in its count nursing homes, assisted living facilities, memory care institutions, retirement communities, and long-term rehabilitation facilities. While these are all defined and regulated somewhat differently, the deaths and illnesses present one of the negative factors of congregate living of older people close together. Perhaps these people would have lived longer lives at a higher quality of life in a different setting. Now, by April 18, 3 days later, the total is 6,900. “Over all, about a fifth of death from the virus in the United States have been tied to nursing homes or other long-term care facilities, The Times review of cases shows.” Today, April 23, 2020, deaths climb to over 10,000.
These deaths demonstrate one of the many reasons to take steps early in your maturity to avoid spending the last year of your life in a nursing home. Now, I’d best get back to writing that book!
Each day I nag myself to work on the book I’m writing, 7 Actions to Take to Stay OUT of a Nursing Home. The coronavirus has pulled a plague on us, and staying out of a nursing home seems even more relevant and yet less relevant than ever in my life and in your life.
Nursing homes are one of the epicenters of the virus. In Kirkland, 20 miles away, the Life Care Center of Kirkland had some of the first diagnoses and many of the first deaths in the state of Washington. Nursing homes are a perfect petri dish for disease. You have closely packed residents with compromised immune systems. You have staff who are often poorly compensated, sometimes minimally trained, and everyone is in close contact providing the most intimate of services.
So, for the time being I am going to focus my writing on aspects of the virus that others are not highlighting and about which I have some expertise.
Are you shut in with a beloved family member with Alzheimer’s? Are you trying to support a cognitively-impaired neighbor living alone? Is your mom in an institution and you are now forbidden to visit?
One of the hardest issues for me with my difficult demented dad was not pointing out how wrong he was. When he tried to give away my mother’s pearls to a caregiver, she properly refused and told me. (Not all caregivers would be so ethical, I know). Rather than preaching that family heirlooms were not an appropriate gift, or that he should not be sexually attracted to his caregiver (which he was), I asked, “Tell me about when you and mom picked out this gorgeous necklace.” He happily complied and we agreed to safeguard it in the box at the bank.
When a person with impaired judgement wants to drive, don’t say, “You are no longer a safe driver.” This is an insult to almost every American, especially a man. Ask instead, “Dad, tell me about your first car.” Or when you learned to drive. Or how you got your first driver’s license. Long-term memory stays intact long after short-term memory is shot. Most individuals with dementia can tell you about their wedding in the 40s but are clueless about what he or she did yesterday.
When mom asks, “Where’s Dad?” never say “Don’t you remember, he died last year?” This is cruel indeed. Ask instead, “Tell me about when you met dad.” Or ask about the wedding or point to the ring and ask when they bought it.
We are accustomed to asking, “What do you want to wear?” or “What do you want to eat?” While choices are honoring preferences are enormously important, simplify. “Do you want to wear the blue shirt or the plaid shirt”, and hold them up. Ask, “Do you want fish or chicken?” This honors control, choice and preferences but doesn’t make it an ordeal of dithering.
Supporting an institutionalized elder is going to be much more difficult during the coronavirus. Since you can’t visit, ponder the other possibilities. I’ve been exchanging postcards with a family member. As long as we still have the sacred postal system, a letter or card can brighten the day for the receiver. It also shows staff that the person they care for is valued. It also is a meaningful activity for you.
If the tools and skills are available, video chatting with Facetime or Zoom are great. Staff are usually willing to help, especially if it is as simple as handing over a cell phone. A phone call, even without the visuals, is communication but of course not every person with dementia can handle it.
Sending flowers may be an option, depending on where you live. Talking with staff will also help you learn what’s going on with the person living there, and it’s an opportunity to thank them for their invaluable service. At the present time, many of the people working in nursing homes, or any health care facility, are risking their lives. Let’s hope they don’t make the ultimate sacrifice and die, as many providers already have.